With emerging interest in the therapeutic potential of psychedelics, combined with regulatory agencies’ renewed interest in targeted central nervous system (CNS) interventions, the purpose of this blog is to provide a broad overview of psychedelics that are currently under investigation for various CNS indications, as well as their intrinsic pharmacology that makes these compounds increasingly interesting in the drug development landscape.
Psychedelics and Their Emerging Role in Treating CNS Indications
The term “psychedelic” is defined by two major components: the first, is that a psychedelic compound can produce a “capacity for allowing greater access to the psyche”; the second is that psychedelic compounds, either through direct modulation or indirect modulation, produce alterations in the serotonin 2 subtype A receptor (5HT2A). Not to be confused with the term “hallucinogen” which is any compound that can induce perceptual alterations (visual or auditory hallucinations, for example), many hallucinogens do not confer a therapeutic potential, but several psychedelics do demonstrate therapeutic potential in addition to inducing perceptual alterations at certain dose levels.
The three main psychedelics currently under investigation for various CNS indications include lysergic acid diethylamide (LSD; “acid”), psilocybin (“mushrooms”), and methylenedioxymethamphetamine (MDMA; “ecstasy”). In the following sections, we will go into detail regarding the specific pharmacology of each of these compounds, as well as the current CNS indications under which they are being investigated.
Understanding the Mechanisms of Action of Psychedelics
Psychedelics demonstrate a unique pharmacology, including interactions with the 5HT2A receptor as outlined above, in addition to other distinct mechanisms of action (MOA) that are specific to the psychedelic under investigation. This section explores the key MOA for LSD, psilocybin, and MDMA, highlighting their unique interactions with neurotransmitter receptors.
LSD
- Defined as a “classical” psychedelic, LSD exerts its potential therapeutic effects via 5HT2A receptor activation. (Titeler et al., 1988)
- Additionally, LSD also interacts with the dopamine 2 receptor (D2). (Watts et al., 1995)
- Currently, LSD is being investigated as a potential therapeutic for cluster headaches in Switzerland
Psilocybin
- Like LSD, psilocybin is also a classical psychedelic, with direct activation of the 5HT2A receptor. (Nichols 2012)
- When psilocybin is consumed, the molecule is metabolized and produces psilocin, which is the compound that induces the majority of biological and behavioral effects ascribed to psilocybin (Fantegrossi et al., 2008).
- Unlike LSD, psilocin/psilocybin does not demonstrate direct dopaminergic activation at either D1 or D2 receptors. (Coull et al., 2011)
- Currently, psilocin/psilocybin is under investigation for numerous CNS indications, including but not limited to:
- Post-traumatic stress disorder (PTSD), obsessive-compulsive disorder (OCD), methamphetamine use disorder, and opioid use disorder in the United States and other countries.
MDMA
- Although some of MDMA’s pharmacology includes modulation of the 5HT2A receptor, MDMA is not considered a classical hallucinogen because it does not directly activate the 5HT2A receptor. Instead, MDMA acts as a monoamine-releasing agent, acting to increase dopaminergic, serotonergic, and noradrenergic release. (Baumann et al., 2007; Fantegrossi et al., 2009)
- Currently, MDMA is under investigation for the treatment of PTSD and alcohol use disorder.
Current Investigation of Psychedelics for Depression, Anxiety, and PTSD
- The FDA recently rejected Lykos Therapeutic’s NDA application for the use of midomafetamine (MDMA) in combination with psychotherapy for the treatment of PTSD in adults based on the conclusion that the product was not an effective treatment for PTSD and its risks outweigh the expected benefits (Reardon, 2024).
- Although the FDA’s rejection underscores the extremely complicated regulatory landscape in examining psychedelics for the treatment of many CNS indications, there is still significant interest in developing psychedelics as therapeutics given that at least twenty Phase 2 studies and seven Phase 3 studies are currently recruiting patients in the United States.
- See Table 1 below for summary information for Phase 3 studies conducted by either academic, government, or commercial entities to evaluate Psilocybin and MDMA under different dose schedules in patients.
- The listed studies and others are targeting the treatment of CNS-related disorders that include PTSD, Adjustment Disorder, Major Depressive Disorder, Treatment-Resistant Depression (TRD), Anxiety, Existential Distress, and Alcohol Use Disorder.
- These studies typically include psychotherapy in combination with drug treatment in patients administered either single or multiple treatments of product separated by multiple weeks.
Table 1. Phase 3 studies designed to evaluate either psilocybin or MDMA in studies currently recruiting patients in the United States
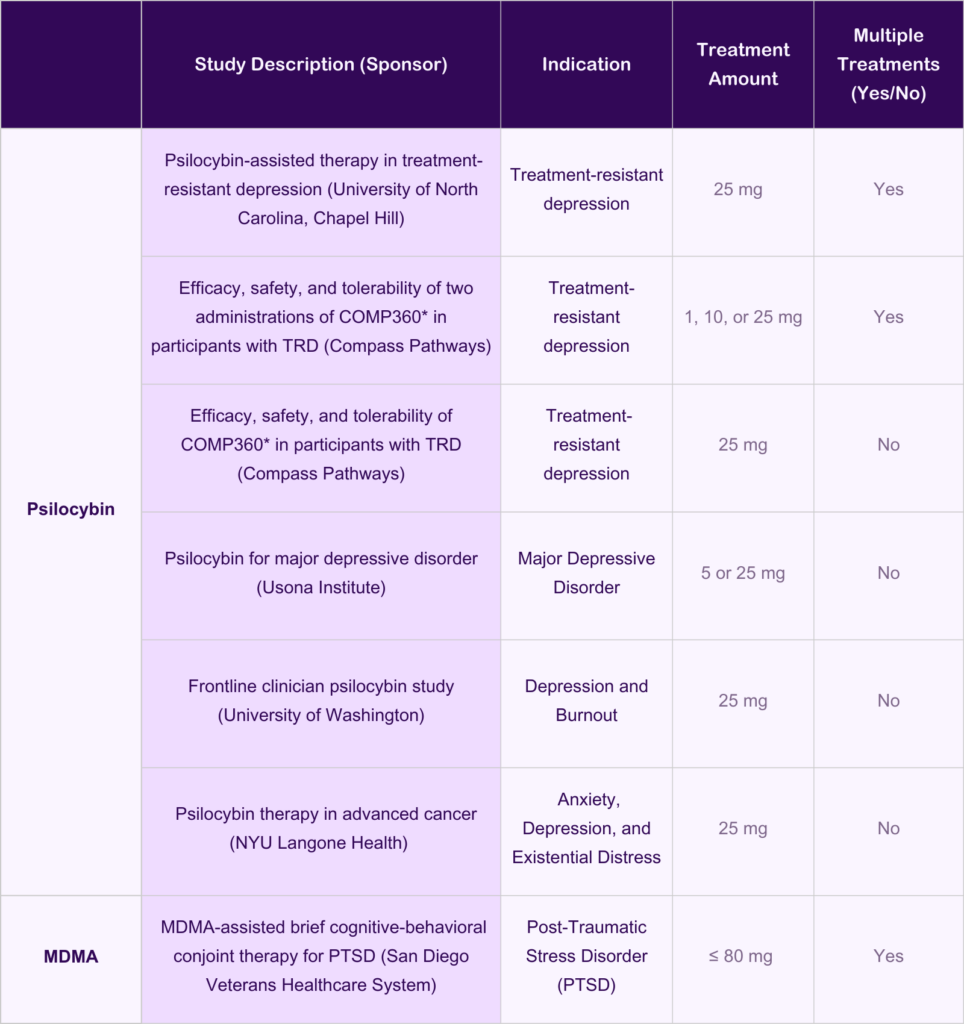
The information included in this table was obtained from ClinicalTrials.gov.
Psilocybin-assisted therapy in treatment-resistant depression
Efficacy, safety, and tolerability of two administrations of COMP360* in participants with TRD
Efficacy, safety, and tolerability of COMP360 in participants with TRD
Psilocybin for major depressive disorder
Frontline clinician psilocybin study
Psilocybin therapy in advanced cancer
MDMA-assisted brief cognitive-behavioral conjoint therapy for PTSD
The Future of Psychedelics in CNS Treatment Approaches
The potential for psychedelics in treating CNS indications is rapidly evolving. As ongoing research continues to unveil the therapeutic benefits of compounds like LSD, psilocybin, and MDMA, it becomes increasingly clear that these therapies may offer new avenues for addressing conditions traditionally seen as challenging to treat. Emerging studies indicate that psychedelics could play a crucial role in not only alleviating symptoms of depression, anxiety, and PTSD but also in enhancing the overall therapeutic landscape for various CNS conditions. The integration of psychedelics into mainstream treatment protocols holds the promise of revolutionizing patient care, providing innovative strategies that are rooted in both clinical evidence and patient-centric approaches.
At Allucent, we are at the forefront of this exciting field with comprehensive expertise in psychedelics and CNS therapies. Our A-Team of experts not only maintain comprehensive and robust knowledge in multiple CNS indications, such as substance use disorders, anxiety and depression disorders, and psychiatric indications related to social behavior, but many are also former FDA reviewers and experts in psychedelic pharmacology and toxicology (Winsauer et al., 2002; Winsauer et al., 2004). For additional related information, you may be interested in reading “Anti-Depression Medication: Current Landscape and Product Development Trends”, or watching our recent webinar, “Risk Assessment of Novel Neurotherapeutics: Mechanistic Translation of Preclinical Safety and PK/PD Data to a Clinical Setting”.
Bibliography
Baumann MH, Wang X, Rothman RB. 3,4-Methylenedioxymethamphetamine (MDMA) neurotoxicity in rats: a reappraisal of past and present findings. Psychopharmacology (Berl). 2007 Jan;189(4):407-24.
Coull JT, Cheng RK, Meck WH. Neuroanatomical and neurochemical substrates of timing. Neuropsychopharmacology. 2011;36(1):3-25.
Fantegrossi WE, Murnane KS, Reissig CJ. The behavioral pharmacology of hallucinogens. Biochem Pharmacol. 2008;75(1):17-33.
Fantegrossi WE, Murai N, Mathúna BO, Pizarro N, de la Torre R. Discriminative stimulus effects of 3,4-methylenedioxymethamphetamine and its enantiomers in mice: pharmacokinetic considerations. J Pharmacol Exp Ther. 2009 Jun;329(3):1006-15.
Nichols, D.E. (2012), Structure–activity relationships of serotonin 5-HT2A agonists. WIREs Membr Transp Signal, 1: 559-579
Reardon S (2024) MDMA therapy for PTSD rejected by FDA panel. Nature.
Titeler M, Lyon RA, Glennon RA. Radioligand binding evidence implicates the brain 5-HT2 receptor as a site of action for LSD and phenylisopropylamine hallucinogens. Psychopharmacology (Berl). 1988;94(2):213-6.
Watts VJ, Lawler CP, Fox DR, Neve KA, Nichols DE, Mailman RB. LSD and structural analogs: pharmacological evaluation at D1 dopamine receptors. Psychopharmacology (Berl). 1995 Apr;118(4):401-9.
Winsauer PJ, McCann UD, Yuan J, Delatte MS, Stevenson MW, Ricaurte GA and Moerschbaecher JM (2002) Effects of fenfluramine, m-CPP and triazolam on repeated-acquisition in squirrel monkeys before and after neurotoxic MDMA administration. Psychopharmacology (Berl) 159:388-396.
Winsauer PJ, Quinton MS, Porter JR, Corll CB, Moerschbaecher JM, Delatte MS, Leonard ST and Stroble SB (2004) Effects of MDMA administration on scopolamine-induced disruptions of learning and performance in rats. Pharmacol Biochem Behav 79:459-472.
